I’m thirty-eight years old. Over the past several years, I have been noticing problems with my mental state that could be described as ADHD. I’ve had trouble with alertness, attention, focus, motivation, executive function, energy levels, mood, and cognition that I didn’t have before at this level; and those things were causing problems in my work life and in my home life. I’m getting treatment now, and while I know that everyone’s brain and experience is different, I’m hopeful that my experience can be helpful to others.
 It was only a year or two ago that I was willing to call this a problem. Growing up in a rural community in the 90s, that diagnosis (well, as ADD) was reserved for students who were doing poorly in school and who were running around all over the classroom; I was doing well academically, and even though I had trouble with focus and attention, I was able to make up for it. I came up with coping strategies, and found things I liked, and simply made it through.
It was only a year or two ago that I was willing to call this a problem. Growing up in a rural community in the 90s, that diagnosis (well, as ADD) was reserved for students who were doing poorly in school and who were running around all over the classroom; I was doing well academically, and even though I had trouble with focus and attention, I was able to make up for it. I came up with coping strategies, and found things I liked, and simply made it through.
In college, the problem compounded as I essentially lost the ability to read long books. I was a voracious reader in high school, but the combination of boring textbooks and a more difficult workload that caused reduced sleep made my brain connect reading with sleep. My coping strategies began to fail, and I found myself struggling more. It took eight years for me to graduate, and I wandered through four different majors in the process. Still, with the development of new coping strategies and the help of my wife (whom I met in 2006 and married in 2010), I was able to graduate and eventually get a job in the tech industry, doing something I enjoyed.
Identifying what was wrong with me became a greater priority a few years into my career, as my family began to grow and my ability to focus on work began to dwindle. It was like I had a certain number of lanes in my brain; and with my work, church, wife, children, and hobbies, there simply wasn’t enough bandwidth to go around.
I first talked to my doctor about this experience a few years ago. He suggested that we rule out other possible issues; things like depression and sleep disorders. First he recommended increasing my activity, so I made it a point to take daily walks or bicycle rides; this worked great to improve my mood and energy levels, but didn’t affect the other issues I was having.
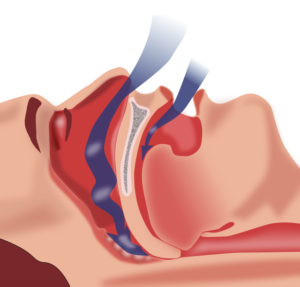 Iterating on the problem, he suggested that I get assessed for a sleep disorder. I did indeed have sleep apnea and began on a CPAP nearly two months ago. While I was cautioned that I probably wouldn’t see immediate results, I actually did: my alertness, motivation, and cognition increased almost immediately. Still no real impact on focus, attention, or executive function, though.
Iterating on the problem, he suggested that I get assessed for a sleep disorder. I did indeed have sleep apnea and began on a CPAP nearly two months ago. While I was cautioned that I probably wouldn’t see immediate results, I actually did: my alertness, motivation, and cognition increased almost immediately. Still no real impact on focus, attention, or executive function, though.
Independent of my own journey, my children were also being assessed for potential ADHD. While filling out the assessment paperwork for my oldest two children, I noticed a lot of things that not only apply to me now, but also would’ve applied to me as a child. What are the odds that a disorder which runs in the family would show up in at least two of my children (and maybe more) but not in myself or my wife? So I made an appointment to follow up on the treatment.
In that appointment, I laid out essentially everything I noted above. The nurse practitioner performed a similar assessment on me to the one that I had filled out for my children, and noted that while I scored high for ADHD, I scored low for depression and anxiety. When diagnosing the disorder, she said, the usual process is to identify the symptoms and then make sure that they couldn’t be explained by anything else; and that our previous attempts to solve the problem with exercise and better sleep indicated that ADHD medication could be a good next step.
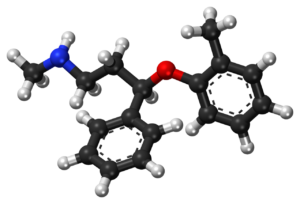
It was there that we encountered another problem, though. See, it is mid-2023 as I write this, and there’s a nationwide medication shortage for ADHD stimulant medication (such as Adderall). The Adderall shortage in particular is making other stimulant medications more scarce, leaving only very expensive non-generic stimulants behind. So we made the decision to begin our medication attempts with a drug called Atomoxetine (the generic name for Strattera), a Selective Norepinephrine Reuptake Inhibitor (sNRI) which reduces the brain’s removal of norepinephrine, the neurotransmitter that mobilizes the brain and body for action. sNRIs are related to SSRIs like Prozac and Zoloft, and are also classified as antidepressants, but are FDA-approved for adult ADHD treatment. We began with a low dose of 40mg, with the understanding that seeing the full results would probably take a few weeks.
 I took the first dose this morning.
I took the first dose this morning.
Initially, I didn’t notice any changes. About an hour after I took the medicine, my brain felt “warm;” not in a bad way, per se, but in a way that felt like it was using more energy.
In the hour after that, my brain activity started to feel “smoother.” I’m not entirely sure how else to characterize it. While I would ordinarily experience sharp spikes in mental activity, motivation, and reward, it felt more regulated. The experience was noticeable, but not game-changing.
It felt in the hour after that like my brain had more capacity; like the lanes that I had were operating at a higher rate, or maybe that there was another lane. And the fact that I’ve written this entire blog post in one sitting (and intentionally begun every paragraph with the letter “I”) either means that my focus is better or I’ve found a new hyperfixation.
I can tell that there are changes going on in my brain, but I don’t know whether they’re good ones or not; and I don’t know what effects are the medication and what are placebo. Still, I’m willing to follow along with it for at least another day or so.
I hope that this account of my experience was helpful to someone. I’ll continue documenting this journey here and on Mastodon.




